Practical Recommendations for Diagnosis and Management of Respiratory Muscle Weakness in Late-Onset Pompe Disease
Abstract
:1. Introduction
2. Background
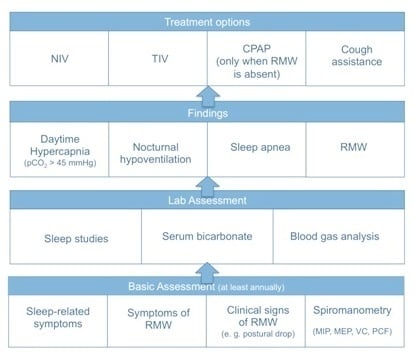
3. Assessment of Respiratory Muscle Function
3.1. Clinical Presentation
3.2. Screening Questionnaires
3.3. Clinical Examination
3.4. Measurement of Respiratory Muscle Function
3.4.1. Pulmonary Function Tests (PFTs)
3.4.2. Peak Cough Flow (PCF)
3.4.3. Manometry
3.4.4. Non-Volitional Tests
3.5. Sleep Studies
3.6. Daytime Blood Gas Analysis
4. Management
4.1. Mechanical Ventilation
4.1.1. Non-Invasive Ventilation (NIV)
4.1.2. Tracheostomy Invasive Ventilation (TIV)
4.2. Respiratory Muscle Training
4.3. Cough Assistance
4.4. Management of Acute Respiratory Failure
4.5. Additional Recommendations
4.5.1. Immunizations
4.5.2. Obstructive Sleep Apnea
4.5.3. Concomitant Pulmonary Disease
4.5.4. Perioperative Management
4.5.5. Scoliosis
4.5.6. Nutrition
4.5.7. Chronic Pain
4.5.8. Palliative Care
4.5.9. Patient and Caregiver Education
5. Methods
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| ARF | Acute respiratory failure |
| BE | Base excess |
| BIPAP | Bilevel inspiratory positive airway pressure |
| CO2 | Carbon dioxide |
| COPD | Chronic obstructive pulmonary disease |
| CPAP | Continuous positive airway pressure |
| ERT | Enzyme replacement therapy |
| ERV | Expiratory reserve volume |
| FVC | Forced vital capacity |
| GAA | α-1,4-glucosidase |
| HFCWO | High frequency chest wall oscillation |
| IC | Inspiratory capacity |
| ICU | Intensive care unit |
| I/E | Insufflation/exsufflation |
| IPV | Intrapulmonary percussive ventilation |
| IRV | Inspiratory reserve volume |
| IVC | Inspiratory vital capacity |
| LOPD | Late-onset Pompe disease |
| MAC | Manually assisted coughing |
| MEP | Maximum expiratory pressure |
| MIP | Maximum inspiratory pressure |
| NIV | Non-invasive ventilation |
| NMD | Neuromuscular disorders |
| OSA | Obstructive sleep apnea |
| PCF | Peak cough flow |
| pCO2 | Carbon dioxide tension |
| PFT | Pulmonary function testing |
| Pdi | Twitch diaphragmatic pressure |
| Pmo | Twitch mouth pressure |
| PO | Pulse oximetry |
| PSG | Polysomnography |
| REM | Rapid eye movement |
| RICU | Respiratory intermediate care unit |
| RMW | Respiratory muscle weakness |
| RMST | Respiratory muscle strength training |
| RMT | Respiratory muscle training |
| RV | Residual volume |
| SaO2 | Arterial oxygen saturation |
| SDB | Sleep-disordered breathing |
| SNIP | Sniff nasal inspiratory pressure |
| SpO2 | Peripheral oxygen saturation |
| SVC | Slow vital capacity |
| tcCO2 | Transcutaneous carbon dioxide tension |
| TLC | Total lung capacity |
| TV | Tidal volume |
| VC | Vital capacity |
References
- Barba-Romero, M.A.; Barrot, E.; Bautista-Lorite, J.; Gutierrez-Rivas, E.; Illa, I.; Jimenez, L.M.; Ley-Martos, M.; Lopez de Munain, A.; Pardo, J.; Pascual-Pascual, S.I.; et al. Clinical guidelines for late-onset Pompe disease. Rev. Neurol. 2012, 54, 497–507. [Google Scholar] [PubMed]
- Bembi, B.; Cerini, E.; Danesino, C.; Donati, M.A.; Gasperini, S.; Morandi, L.; Musumeci, O.; Parenti, G.; Ravaglia, S.; Seidita, F.; et al. Management and treatment of glycogenosis type II. Neurology 2008, 71 (Suppl. 2), S12–S36. [Google Scholar] [CrossRef] [PubMed]
- Cupler, E.J.; Berger, K.I.; Leshner, R.T.; Wolfe, G.I.; Han, J.J.; Barohn, R.J.; Kissel, J.T. Consensus treatment recommendations for late-onset Pompe disease. Muscle Nerve 2012, 45, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Kishnani, P.S.; Steiner, R.D.; Bali, D.; Berger, K.; Byrne, B.J.; Case, L.E.; Crowley, J.F.; Downs, S.; Howell, R.R.; Kravitz, R.M.; et al. Pompe disease diagnosis and management guideline. Genet. Med. 2006, 8, 267–288. [Google Scholar] [CrossRef] [PubMed]
- Ambrosino, N.; Confalonieri, M.; Crescimanno, G.; Vianello, A.; Vitacca, M. The role of respiratory management of Pompe disease. Respir. Med. 2013, 107, 1124–1132. [Google Scholar] [CrossRef] [PubMed]
- Poorthuis, B.J.; Wevers, R.A.; Kleijer, W.J.; Groener, J.E.; de Jong, J.G.; van Weely, S.; Niezen-Koning, K.E.; van Diggelen, O.P. The frequency of lysosomal storage diseases in The Netherlands. Hum. Genet. 1999, 105, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Filosto, M.; Todeschini, A.; Cotelli, M.S.; Vielmi, V.; Rinaldi, F.; Rota, S.; Scarpelli, M.; Padovani, A. Non-muscle involvement in late-onset glycogenosis II. Acta Myol. 2013, 32, 91–94. [Google Scholar] [PubMed]
- Kishnani, P.S.; Corzo, D.; Nicolino, M.; Byrne, B.; Mandel, H.; Hwu, W.L.; Leslie, N.; Levine, J.; Spencer, C.; McDonald, M.; et al. Recombinant human acid α-glucosidase: Major clinical benefits in infantile-onset Pompe disease. Neurology 2007, 68, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Hagemans, M.L.; Winkel, L.P.; van Doorn, P.A.; Hop, W.J.; Loonen, M.C.; Reuser, A.J.; van der Ploeg, A.T. Clinical manifestation and natural course of late-onset Pompe’s disease in 54 Dutch patients. Brain 2005, 128, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Prigent, H.; Orlikowski, D.; Laforet, P.; Letilly, N.; Falaize, L.; Pellegrini, N.; Annane, D.; Raphael, J.C.; Lofaso, F. Supine volume drop and diaphragmatic function in adults with Pompe disease. Eur. Respir. J. 2012, 39, 1545–1546. [Google Scholar] [CrossRef] [PubMed]
- Gaeta, M.; Barca, E.; Ruggeri, P.; Minutoli, F.; Rodolico, C.; Mazziotti, S.; Milardi, D.; Musumeci, O.; Toscano, A. Late-onset Pompe disease (LOPD): Correlations between respiratory muscles CT and MRI features and pulmonary function. Mol. Genet. Metab. 2013, 110, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Berger, K.I.; Chan, Y.; Rom, W.N.; Oppenheimer, B.W.; Goldring, R.M. Progression from respiratory dysfunction to failure in late-onset Pompe disease. Neuromuscul. Disord. 2016, 26, 481–489. [Google Scholar] [CrossRef] [PubMed]
- Falk, D.J.; Todd, A.G.; Lee, S.; Soustek, M.S.; ElMallah, M.K.; Fuller, D.D.; Notterpek, L.; Byrne, B.J. Peripheral nerve and neuromuscular junction pathology in Pompe disease. Hum. Mol. Genet. 2015, 24, 625–636. [Google Scholar] [CrossRef] [PubMed]
- DeRuisseau, L.R.; Fuller, D.D.; Qiu, K.; DeRuisseau, K.C.; Donnelly, W.H., Jr.; Mah, C.; Reier, P.J.; Byrne, B.J. Neural deficits contribute to respiratory insufficiency in Pompe disease. Proc. Natl. Acad. Sci. USA 2009, 106, 9419–9424. [Google Scholar] [CrossRef] [PubMed]
- Toscano, A.; Schoser, B. Enzyme replacement therapy in late-onset Pompe disease: A systematic literature review. J. Neurol. 2013, 260, 951–959. [Google Scholar] [CrossRef] [PubMed]
- Van der Ploeg, A.T.; Clemens, P.R.; Corzo, D.; Escolar, D.M.; Florence, J.; Groeneveld, G.J.; Herson, S.; Kishnani, P.S.; Laforet, P.; Lake, S.L.; et al. A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N. Engl. J. Med. 2010, 362, 1396–1406. [Google Scholar] [CrossRef] [PubMed]
- Van der Beek, N.A.; Hagemans, M.L.; Reuser, A.J.; Hop, W.C.; van der Ploeg, A.T.; van Doorn, P.A.; Wokke, J.H. Rate of disease progression during long-term follow-up of patients with late-onset Pompe disease. Neuromuscul. Disord. 2009, 19, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Regnery, C.; Kornblum, C.; Hanisch, F.; Vielhaber, S.; Strigl-Pill, N.; Grunert, B.; Muller-Felber, W.; Glocker, F.X.; Spranger, M.; Deschauer, M.; et al. 36 months observational clinical study of 38 adult Pompe disease patients under alglucosidase alfa enzyme replacement therapy. J. Inherit. Metab. Dis. 2012, 35, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Boentert, M.; Karabul, N.; Wenninger, S.; Stubbe-Drager, B.; Mengel, E.; Schoser, B.; Young, P. Sleep-related symptoms and sleep-disordered breathing in adult Pompe disease. Eur. J. Neurol. 2015, 22, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, C.M.; Elmes, P.C.; Fairbairn, A.S.; Wood, C.H. The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br. Med. J. 1959, 2, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Kendrick, K.R.; Baxi, S.C.; Smith, R.M. Usefulness of the modified 0–10 Borg scale in assessing the degree of dyspnea in patients with COPD and asthma. J. Emerg. Nurs. 2000, 26, 216–222. [Google Scholar] [CrossRef]
- Steier, J.; Jolley, C.J.; Seymour, J.; Teschler, H.; Luo, Y.M.; Polkey, M.I.; Moxham, J. Screening for sleep-disordered breathing in neuromuscular disease using a questionnaire for symptoms associated with diaphragm paralysis. Eur. Respir. J. 2011, 37, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Van der Beek, N.A.; van Capelle, C.I.; van der Velden-van Etten, K.I.; Hop, W.C.; van den Berg, B.; Reuser, A.J.; van Doorn, P.A.; van der Ploeg, A.T.; Stam, H. Rate of progression and predictive factors for pulmonary outcome in children and adults with Pompe disease. Mol. Genet. Metab. 2011, 104, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Hankinson, J.L.; Odencrantz, J.R.; Fedan, K.B. Spirometric reference values from a sample of the general U.S. population. Am. J. Respir. Crit. Care Med. 1999, 159, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Falaschetti, E.; Laiho, J.; Primatesta, P.; Purdon, S. Prediction equations for normal and low lung function from the Health Survey for England. Eur. Respir. J. 2004, 23, 456–463. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.J.; Pride, N.B.; Davis, J.N.; Loh, L.C. Pulmonary mechanics in patients with respiratory muscle weakness. Am. Rev. Respir. Dis. 1977, 115, 389–395. [Google Scholar] [PubMed]
- Mellies, U.; Ragette, R.; Schwake, C.; Baethmann, M.; Voit, T.; Teschler, H. Sleep-disordered breathing and respiratory failure in acid maltase deficiency. Neurology 2001, 57, 1290–1295. [Google Scholar] [CrossRef] [PubMed]
- Ragette, R.; Mellies, U.; Schwake, C.; Voit, T.; Teschler, H. Patterns and predictors of sleep disordered breathing in primary myopathies. Thorax 2002, 57, 724–728. [Google Scholar] [CrossRef] [PubMed]
- Toussaint, M.; Steens, M.; Soudon, P. Lung function accurately predicts hypercapnia in patients with Duchenne muscular dystrophy. Chest 2007, 131, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Bach, J.R.; Saporito, L.R. Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure. A different approach to weaning. Chest 1996, 110, 1566–1571. [Google Scholar] [CrossRef] [PubMed]
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 2002, 166, 518–624. [Google Scholar]
- Evans, J.A.; Whitelaw, W.A. The assessment of maximal respiratory mouth pressures in adults. Respir. Care 2009, 54, 1348–1359. [Google Scholar] [PubMed]
- Kabitz, H.J.; Walterspacher, S.; Mellies, U.; Criee, C.P.; Windisch, W. Recommendations for respiratory muscle testing. Pneumologie 2014, 68, 307–314. [Google Scholar] [PubMed]
- Prigent, H.; Orlikowski, D.; Fermanian, C.; Lejaille, M.; Falaize, L.; Louis, A.; Fauroux, B.; Lofaso, F. Sniff and Muller manoeuvres to measure diaphragmatic muscle strength. Respir. Med. 2008, 102, 1737–1743. [Google Scholar] [CrossRef] [PubMed]
- Windisch, W.; Kabitz, H.J.; Sorichter, S. Influence of different trigger techniques on twitch mouth pressure during bilateral anterior magnetic phrenic nerve stimulation. Chest 2005, 128, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Boon, A.J.; O’Gorman, C. Ultrasound in the Assessment of Respiration. J. Clin. Neurophysiol. 2016, 33, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Mogalle, K.; Perez-Rovira, A.; Ciet, P.; Wens, S.C.; van Doorn, P.A.; Tiddens, H.A.; van der Ploeg, A.T.; de Bruijne, M. Quantification of Diaphragm Mechanics in Pompe Disease Using Dynamic 3D MRI. PLoS ONE 2016, 11, e0158912. [Google Scholar] [CrossRef] [PubMed]
- Johnson, E.M.; Roberts, M.; Mozaffar, T.; Young, P.; Quartel, A.; Berger, K.I. Pulmonary function tests (maximum inspiratory pressure, maximum expiratory pressure, vital capacity, forced vital capacity) predict ventilator use in late-onset Pompe disease. Neuromuscul. Disord. 2016, 26, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [PubMed]
- Buysse, D.J.; Reynolds, C.F., 3rd; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Krupp, L.B.; LaRocca, N.G.; Muir-Nash, J.; Steinberg, A.D. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch. Neurol. 1989, 46, 1121–1123. [Google Scholar] [CrossRef] [PubMed]
- Hukins, C.A.; Hillman, D.R. Daytime predictors of sleep hypoventilation in Duchenne muscular dystrophy. Am. J. Respir. Crit. Care Med. 2000, 161, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Kushida, C.A.; Littner, M.R.; Morgenthaler, T.; Alessi, C.A.; Bailey, D.; Coleman, J., Jr.; Friedman, L.; Hirshkowitz, M.; Kapen, S.; Kramer, M.; et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep 2005, 28, 499–521. [Google Scholar] [PubMed]
- Mokhlesi, B.; Tulaimat, A.; Faibussowitsch, I.; Wang, Y.; Evans, A.T. Obesity hypoventilation syndrome: Prevalence and predictors in patients with obstructive sleep apnea. Sleep Breath. 2007, 11, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, Y.; Miura, T.; Ishikawa, Y.; Aoyagi, T.; Ogata, H.; Hamada, S.; Minami, R. Duchenne muscular dystrophy: survival by cardio-respiratory interventions. Neuromuscul. Disord. 2011, 21, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Kansagra, S.; Austin, S.; DeArmey, S.; Kazi, Z.; Kravitz, R.M.; Kishnani, P.S. Longitudinal polysomnographic findings in infantile Pompe disease. Am. J. Med. Genet. A 2015, 167, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Kansagra, S.; Austin, S.; DeArmey, S.; Kishnani, P.S.; Kravitz, R.M. Polysomnographic findings in infantile Pompe disease. Am. J. Med. Genet. A 2013, 161, 3196–3200. [Google Scholar] [CrossRef] [PubMed]
- Mellies, U.; Stehling, F.; Dohna-Schwake, C.; Ragette, R.; Teschler, H.; Voit, T. Respiratory failure in Pompe disease: Treatment with noninvasive ventilation. Neurology 2005, 64, 1465–1467. [Google Scholar] [CrossRef] [PubMed]
- Norman, R.G.; Goldring, R.M.; Clain, J.M.; Oppenheimer, B.W.; Charney, A.N.; Rapoport, D.M.; Berger, K.I. Transition from acute to chronic hypercapnia in patients with periodic breathing: Predictions from a computer model. J. Appl. Physiol. 2006, 100, 1733–1741. [Google Scholar] [CrossRef] [PubMed]
- Levine, S.; Nguyen, T.; Taylor, N.; Friscia, M.E.; Budak, M.T.; Rothenberg, P.; Zhu, J.; Sachdeva, R.; Sonnad, S.; Kaiser, L.R.; et al. Rapid disuse atrophy of diaphragm fibers in mechanically ventilated humans. N. Engl. J. Med. 2008, 358, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- Janssens, J.P.; Borel, J.C.; Pepin, J.L.; SomnoNIVGroup. Nocturnal monitoring of home non-invasive ventilation: The contribution of simple tools such as pulse oximetry, capnography, built-in ventilator software and autonomic markers of sleep fragmentation. Thorax 2011, 66, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Berlowitz, D.J.; Tamplin, J. Respiratory muscle training for cervical spinal cord injury. Cochrane Database Syst. Rev. 2013, 7, CD008507. [Google Scholar] [PubMed]
- Illi, S.K.; Held, U.; Frank, I.; Spengler, C.M. Effect of respiratory muscle training on exercise performance in healthy individuals: A systematic review and meta-analysis. Sports Med. 2012, 42, 707–724. [Google Scholar] [CrossRef] [PubMed]
- Winkler, G.; Zifko, U.; Nader, A.; Frank, W.; Zwick, H.; Toifl, K.; Wanke, T. Dose-dependent effects of inspiratory muscle training in neuromuscular disorders. Muscle Nerve 2000, 23, 1257–1260. [Google Scholar] [CrossRef]
- Jones, H.N.; Crisp, K.D.; Moss, T.; Strollo, K.; Robey, R.; Sank, J.; Canfield, M.; Case, L.E.; Mahler, L.; Kravitz, R.M.; et al. Effects of respiratory muscle training (RMT) in children with infantile-onset Pompe disease and respiratory muscle weakness. J. Pediatr. Rehabil. Med. 2014, 7, 255–265. [Google Scholar] [PubMed]
- Jones, H.N.; Crisp, K.D.; Robey, R.R.; Case, L.E.; Kravitz, R.M.; Kishnani, P.S. Respiratory muscle training (RMT) in late-onset Pompe disease (LOPD): Effects of training and detraining. Mol. Genet. Metab. 2016, 117, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Jones, H.N.; Moss, T.; Edwards, L.; Kishnani, P.S. Increased inspiratory and expiratory muscle strength following respiratory muscle strength training (RMST) in two patients with late-onset Pompe disease. Mol. Genet. Metab. 2011, 104, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Jevnikar, M.; Kodric, M.; Cantarutti, F.; Cifaldi, R.; Longo, C.; Della Porta, R.; Bembi, B.; Confalonieri, M. Respiratory muscle training with enzyme replacement therapy improves muscle strength in late—Onset Pompe disease. Mol. Genet. Metabol. Rep. 2015, 5, 67–71. [Google Scholar]
- Estrup, C.; Lyager, S.; Noeraa, N.; Olsen, C. Effect of respiratory muscle training in patients with neuromuscular diseases and in normals. Respiration 1986, 50, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Rassler, B.; Hallebach, G.; Kalischewski, P.; Baumann, I.; Schauer, J.; Spengler, C.M. The effect of respiratory muscle endurance training in patients with myasthenia gravis. Neuromuscul. Disord. 2007, 17, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Bach, J.R. Mechanical insufflation-exsufflation. Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest 1993, 104, 1553–1562. [Google Scholar] [CrossRef] [PubMed]
- Feigelson, C.I.; Dickinson, D.G.; Talner, N.S.; Wilson, J.L. Glossopharyngeal breathing as an aid to the coughing mechanism in the patient with chronic poliomyelitis in a respirator. N. Engl. J. Med. 1956, 254, 611–613. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.A. Physiotherapy for airway clearance in adults. Eur. Respir. J. 1999, 14, 1418–1424. [Google Scholar] [CrossRef] [PubMed]
- Tzeng, A.C.; Bach, J.R. Prevention of pulmonary morbidity for patients with neuromuscular disease. Chest 2000, 118, 1390–1396. [Google Scholar] [CrossRef] [PubMed]
- Toussaint, M.; de Win, H.; Steens, M.; Soudon, P. Effect of intrapulmonary percussive ventilation on mucus clearance in duchenne muscular dystrophy patients: A preliminary report. Respir. Care 2003, 48, 940–947. [Google Scholar] [PubMed]
- Chatburn, R.L. High-frequency assisted airway clearance. Respir. Care 2007, 52, 1224–1235; discussion 1235–1237. [Google Scholar] [PubMed]
- Corrado, A.; Roussos, C.; Ambrosino, N.; Confalonieri, M.; Cuvelier, A.; Elliott, M.; Ferrer, M.; Gorini, M.; Gurkan, O.; Muir, J.F.; et al. European Respiratory Society Task Force on epidemiology of respiratory intermediate care in Europe. Respiratory intermediate care units: A European survey. Eur. Respir. J. 2002, 20, 1343–1350. [Google Scholar] [PubMed]
- Esposito, S.; Passera, S. Vaccination in patients with disorders of the muscle and neuromuscular junction. Expert Rev. Vaccines 2013, 12, 1341–1349. [Google Scholar] [CrossRef] [PubMed]
- Nuckton, T.J.; Glidden, D.V.; Browner, W.S.; Claman, D.M. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep 2006, 29, 903–908. [Google Scholar] [PubMed]
- Carlier, R.Y.; Laforet, P.; Wary, C.; Mompoint, D.; Laloui, K.; Pellegrini, N.; Annane, D.; Carlier, P.G.; Orlikowski, D. Whole-body muscle MRI in 20 patients suffering from late onset Pompe disease: Involvement patterns. Neuromuscul. Disord. 2011, 21, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Dubrovsky, A.; Corderi, J.; Lin, M.; Kishnani, P.S.; Jones, H.N. Expanding the phenotype of late-onset Pompe disease: Tongue weakness: A new clinical observation. Muscle Nerve 2011, 44, 897–901. [Google Scholar] [CrossRef] [PubMed]
- Ing, R.J.; Cook, D.R.; Bengur, R.A.; Williams, E.A.; Eck, J.; Dear Gde, L.; Ross, A.K.; Kern, F.H.; Kishnani, P.S. Anaesthetic management of infants with glycogen storage disease type II: A physiological approach. Paediatr. Anaesth. 2004, 14, 514–519. [Google Scholar] [CrossRef] [PubMed]
- McFarlane, H.J.; Soni, N. Pompe’s disease and anaesthesia. Anaesthesia 1986, 41, 1219–1224. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.S.; Cho, A.R.; Hong, J.M.; Kim, E.S.; Park, S.C.; Yoon, J.Y.; Kim, T.K. Combined general and epidural anesthesia for major abdominal surgery in a patient with Pompe disease. J. Anesth. 2010, 24, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.; Kishnani, P.S.; van der Ploeg, A.T.; Muller-Felber, W.; Merlini, L.; Prasad, S.; Case, L.E. The prevalence and impact of scoliosis in Pompe disease: Lessons learned from the Pompe Registry. Mol. Genet. Metab. 2011, 104, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Schuller, A.; Wenninger, S.; Strigl-Pill, N.; Schoser, B. Toward deconstructing the phenotype of late-onset Pompe disease. Am. J. Med. Genet. Part C 2012, 160, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Haaker, G.; Forst, J.; Forst, R.; Fujak, A. Orthopedic management of patients with Pompe disease: A retrospective case series of 8 patients. Sci. World J. 2014, 2014, 963861. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Shimada, Y.; Ikegami, M.; Kawai, T.; Sakurai, K.; Urashima, T.; Ijima, M.; Fujiwara, M.; Kaneshiro, E.; Ohashi, T.; et al. Prognostic factors for the late onset Pompe disease with enzyme replacement therapy: From our experience of 4 cases including an autopsy case. Mol. Genet. Metab. 2010, 100, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Teichtahl, H.; Wang, D. Sleep-disordered breathing with chronic opioid use. Expert Opin. Drug Saf. 2007, 6, 641–649. [Google Scholar] [CrossRef] [PubMed]

| Test | Device/Method | LLN | Significance | Recommendations |
|---|---|---|---|---|
| MEP | Manometer | Females 70 cm H2O, males 100 cm H2O | Expiratory muscle strength | First-line, at least annually |
| PCF | Peak flow meter | 270 L/min, airway clearance impaired if 160–270 L/min, airway clearance impossible if <160 L/min | Reduced vital capacity Reduced inspiratory and expiratory muscle strength | First-line, at least annually widely available |
| MIP | Manometer | Females 70 cm H2O, males 80 cm H2O | Inspiratory muscle strength | First-line, at least annually |
| SNIP | Manometer | Females 60 cm H2O, males 70 cm H2O | Inspiratory muscle strength | Surrogate of MIP if weakness of the orbicularis oris muscle is present |
| VC | Spirometry | Upright > 80% of predicted VC, supine > 80% of upright VC | IRV + TV + ERV (global test of lung volume and respiratory muscle performance) | First-line, at least annually |
| Mode | Non-Invasive Ventilation (NIV) | Invasive Ventilation (IV/TIV) |
|---|---|---|
| Indications |
|
|
| and at least one of the following: | ||
| ||
| Contraindications | Relative |
|
| ||
| Absolute | ||
|
| Symptoms | Mucus obstruction, recurrent desaturations, recurrent pulmonary infections | |
| Testing | PCF, MEP | |
| When to start |
| |
| Techniques | MAC |
|
| Air stacking |
| |
| I/E |
| |
| HFCWO |
| |
| Optional measures | Mucolysis | Hydration, mucolytics (with caution) |
| Suction | If expectoration cannot be achieved by MAC, I/E, HFCWO alone | |
|
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boentert, M.; Prigent, H.; Várdi, K.; Jones, H.N.; Mellies, U.; Simonds, A.K.; Wenninger, S.; Barrot Cortés, E.; Confalonieri, M. Practical Recommendations for Diagnosis and Management of Respiratory Muscle Weakness in Late-Onset Pompe Disease. Int. J. Mol. Sci. 2016, 17, 1735. https://doi.org/10.3390/ijms17101735
Boentert M, Prigent H, Várdi K, Jones HN, Mellies U, Simonds AK, Wenninger S, Barrot Cortés E, Confalonieri M. Practical Recommendations for Diagnosis and Management of Respiratory Muscle Weakness in Late-Onset Pompe Disease. International Journal of Molecular Sciences. 2016; 17(10):1735. https://doi.org/10.3390/ijms17101735
Chicago/Turabian StyleBoentert, Matthias, Hélène Prigent, Katalin Várdi, Harrison N. Jones, Uwe Mellies, Anita K. Simonds, Stephan Wenninger, Emilia Barrot Cortés, and Marco Confalonieri. 2016. "Practical Recommendations for Diagnosis and Management of Respiratory Muscle Weakness in Late-Onset Pompe Disease" International Journal of Molecular Sciences 17, no. 10: 1735. https://doi.org/10.3390/ijms17101735